Nearly four years after his patient died following a police altercation, a South Carolina paramedic is publicly questioning ketamine, the sedative he injected into the patient's arm before the man lost consciousness forever.
"I have been deeply depressed, and I have not been able to get back on an ambulance," said Greg Carney, a Charleston County, South Carolina paramedic. "Not a day has gone by in three-and-a-half years, that this hasn't consumed my thoughts."
In 2019, Carney administered ketamine to Jamie Britt, 50, in Mount Pleasant, South Carolina, as police officers held Britt in a prone position during an arrest for public intoxication.
"The goal was to protect the patient and to protect the responders on scene and to help ease his state of combativeness," said Carney. "My thought process was, 'We're helping him by sedating him. That's what we're trained. That's what we were taught. That's what the protocol called for.'"
Britt, a husband and the father of a nine-year-old boy, never regained consciousness.
Nearly two weeks later, he died.
"Based on the turn of events, I would have to question whether or not that's the best drug for that type of scenario," said Carney.
Though South Carolina's Office of the Attorney General concluded there was "insufficient evidence to merit criminal prosecution," the Charleston County Coroner's Office ruled the death a homicide, blaming restraint asphyxia and the toxic effects of ketamine as the causes.
The autopsy also listed other significant conditions including, "hypertensive and atherosclerotic cardiovascular disease," "toxic effects of ethanol," and "obesity," in Britt's diagnosis.
"I would want (the patient's family) to know that I am terribly sorry for their loss, and I mean that with all my heart," said Carney.

More states pushing to allow psychologists to prescribe medicine
Nearly a dozen states have considered authorizing psychologists to write prescriptions, but legislative changes have not happened since 2017.
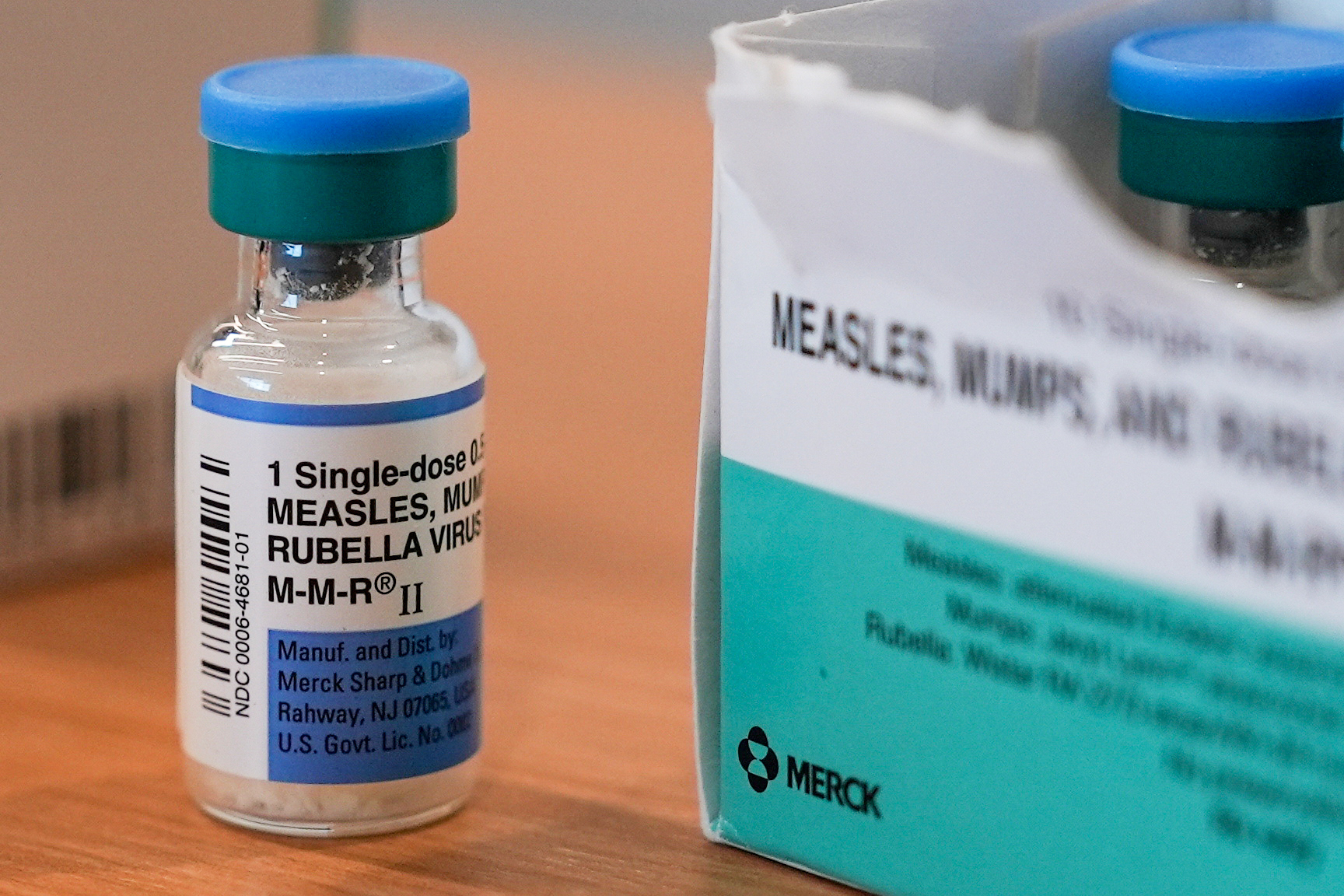
What is ketamine?
Ketamine is a dissociative anesthetic that has been widely used for several decades in various medical treatments.
The drug was approved by the Food and Drug Administration as an intravenous or intramuscular injection solution for "induction and maintenance of general anesthesia," but many medical professionals and researchers have found "off-label" purposes for the medication, including as a method to reduce pain, as a potential treatment for Post-Traumatic Stress Disorder and depression, and as a means of sedating an agitated person outside of a hospital.
According to an exclusive Scripps News survey, agencies in 48 states allow paramedics to utilize ketamine, off-label, to sedate patients who are exhibiting behavioral conditions — like agitation or combativeness — in a pre-hospital setting.
Hawaii and Colorado are the current exceptions.
"I couldn't think of a medicine that I'd rather give in an uncontrolled situation, meaning not on a monitor, not in an intensive care unit," said Dr. Daniel Brooks, a medical toxicologist who serves as medical director of Banner Poison and Drug Information Center in Phoenix, Arizona.
Ketamine has been a "really important drug" to help safely take care of these patients, he said.
"When you don't know what the patient's history is, you know, they're not able to tell you, 'this is my weight; this is my past medical history; this is my cardiac function; these are the four medications that I'm taking at home; this is the illicit drug that I used two hours ago,' when you don't have any of that information, I think it's safest to use the drug that's got the least drug interactions and the least likely to cause acute effects," he said. "And that would be ketamine."
Brooks said the drug is "safe for lots of reasons."
It has "consistently reproduceable or anticipated effects on the blood pressure and heart rate," he explained, and it has a "wide therapeutic index," meaning, the dose someone may receive could vary without adverse effects.
Brooks said there are possible side effects, including laryngospasm. "The musculature in their upper airway can have a bit of a spasm and make it difficult for [a patient] to breathe properly or to swallow," he said. "That's rare, but it can occur." He said, "mild fluctuations in blood pressure and heart rate" can also occur.
Studies published in the Annals of Emergency Medicine in 2021 and the Lancet Regional Health in 2022 examined ketamine administrations outside of a hospital setting, either noting rare patient mortality or that serious adverse events as a result of the sedation were rare.
The 2021 publication featured a study conducted by researchers at ESO that noted 23 percent of agitated patients — or those who received ketamine outside of hospital setting for a behavioral reason — had evidence of at least one episode of decreased respiratory rate.
Both studies emphasized the importance of monitoring a patient after administering the drug.

How effective are anti-depressants?
Many Americans battle depression. How do anti-depressant drugs work, and how effective are they?
Controversial cases
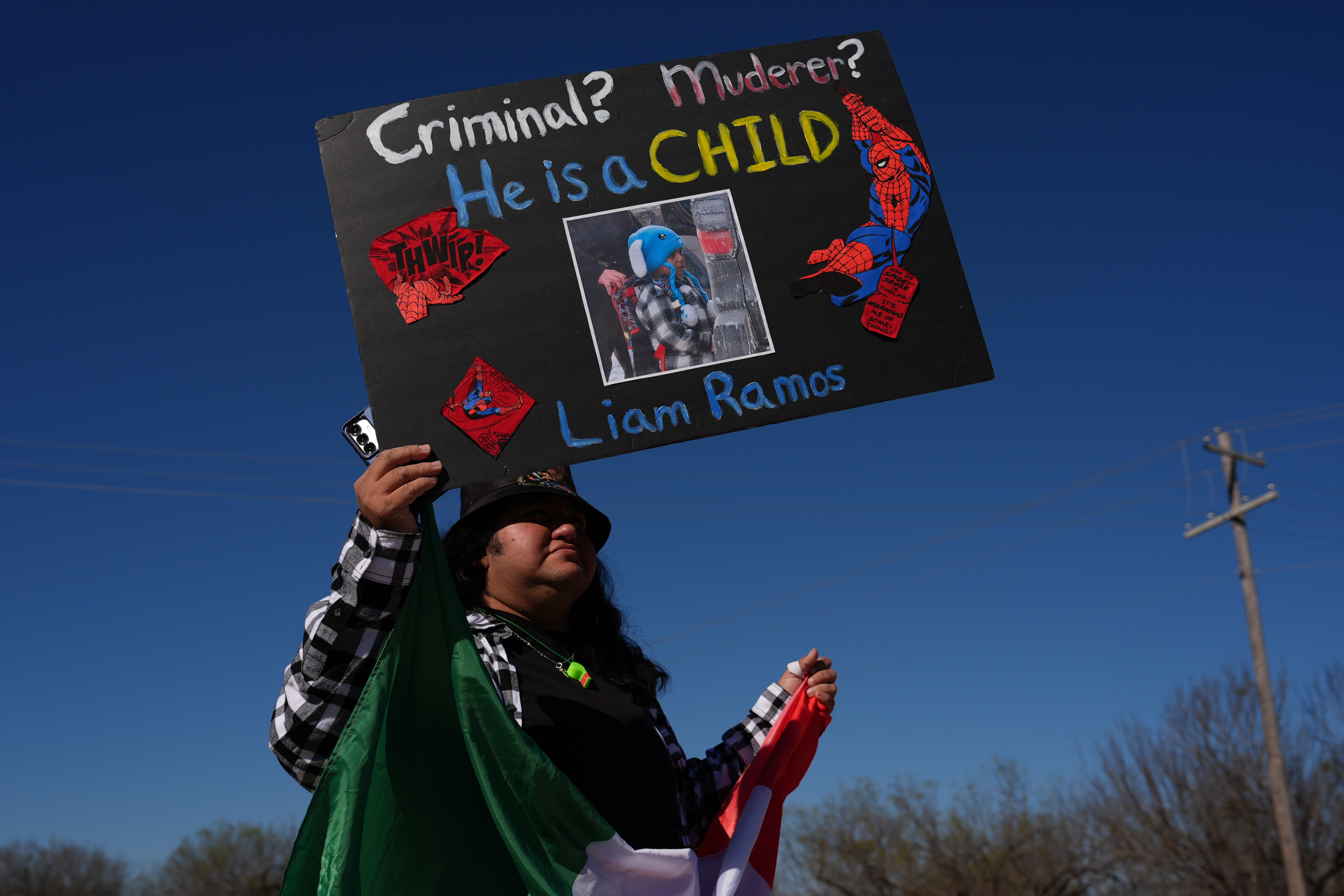
While medical professionals insist the medication has a good safety profile, how the drug has been used in recent years — in scenarios in which a patient is described as agitated or combative — has raised questions among several patients and their loved ones, especially after it was linked to the high-profile death of Elijah McClain.
McClain lost consciousness and later died after a paramedic injected him with ketamine, following a rough police encounter in Aurora, Colorado.
In an amended autopsy, the chief coroner in Adams County, Colorado said McClain died because of "complications of ketamine administration following forcible restraint."
"It is my opinion that he likely would have recovered if he did not receive this injection," Dr. Stephen J. Cina, a forensic pathology consultant who examined the incident for the Adams County Office of the Corner, wrote.
Two paramedics and three police officers pleaded not guilty to criminally negligent homicide and manslaughter charges related to that case.
Following McClain’s death, other patients and families began to question other incidents in which the drug was administered in Colorado — including at least two cases involving a death following an injection; a case in which a man found himself in an intensive care unit after receiving the drug; and others who said a paramedic injected them unnecessarily while they were already physically restrained by police.
In 2021, Colorado enacted a new law and new health policies restricting the purposes for which the drug could be used by paramedics, following McClain’s tragedy.
Currently, Colorado does not allow ketamine administration for agitation in a pre-hospital setting, according to Peter Myers, a public information officer for the Colorado Department of Public Health and Environment, CDPHE.
The state also convened a Ketamine Investigatory Review Panel involving eight medical experts, including the chief medical officer for CDPHE, Dr. Eric France, who led the group.
In late 2021, the panel determined "ketamine is a safe drug if used properly and monitored closely by properly trained and qualified paramedics. However, certain adverse events appear to have arisen primarily from the administration of ketamine and other sedatives to individuals who may not have a medical need for these medications and who could have been managed with a less assertive alternative."

Jamie Britt’s encounter with police and paramedics
"I never even knew that people could use anything like this," said Tabitha Britt, Jamie Britt's widow. "Never in my wildest dreams would I have thought they would inject somebody with something that could potentially kill them," she said.
Her husband, who was 50 when he passed away in October 2019, enjoyed spending time on the South Carolina shore, working on boats and enjoying precious moments with his son.
"We had so many dreams," said Tabitha.
Before the paramedics arrived at her husband's side in September 2019, multiple Mount Pleasant police officers attempted to restrain Britt, who was 6-feet-tall and weighed approximately 300 pounds.
Earlier in the evening, Britt, who had more than three times the legal driving limit of alcohol in his system, had pulled into a Mount Pleasant, SC neighborhood, Snee Farms, after a tire "blew out" on the car he was driving.
A passing motorist called 911 to report that she had seen Britt, who was shirtless, urinating in public.
Police were dispatched to the scene.
The first police officer who approached Britt asked if he needed help with the tire. For the next 17 minutes, other officers arrived on scene, and eventually, a police supervisor told Britt he would be arresting Britt for public intoxication.
A group of officers brought Britt to the ground, where they handcuffed him and placed leg shackles on his ankles.
In police body camera footage, officers called Britt "uncooperative" and said he was resisting arrest as Britt wiggled and shouted profanities.
Britt repeatedly shouted, "Roll me!" as he snorted and begged to be turned on his back for a better breath of air.
By the end of the police altercation, Britt had been held down for nearly 20 minutes, mostly face-down. He received ketamine about 15 minutes after police first placed him in custody.
Legal action
Tabitha Britt sued the Mount Pleasant Police Department and settled in 2020 for $3 million.
She also filed a lawsuit, alleging wrongful death and other related claims, against the paramedics, their employer, Charleston County, and other medical leaders in the county.
In court filings, the defendants denied the allegations of wrongdoing.
The paramedics' involvement
When Greg Carney encountered Britt, he was working with another paramedic, Tom Esdorn, who declined to be interviewed.
Police body camera footage shows Esdorn approaching the scene and calling out to Carney to prepare ketamine for the patient.
"The idea of sedating is to prevent any further injury to the patient and to the first responders on the scene, and to sort of relax the patient," said Carney.
Carney said he believed his patient, at the time, "met the scenario" that allowed for the administration of ketamine based on Charleston County's EMS guidelines in 2019.
A Charleston County spokesperson declined to be interviewed due to the pending lawsuit, but Scripps News obtained the 2019 Charleston County Clinical Operating Guidelines.
The guidelines indicate ketamine may be used if a patient is "clearly a danger to self or others."
The protocol also emphasized, "Crew/responder safety is the main priority."
"The decision was made ... to administer ketamine in a hope to calm the patient, relax the patient, make the scene safe for everyone involved," said Carney. "Based on the limited experience that I have with ketamine administration, I wasn't expecting the turn of events. And we weren't really prepared, from a training standpoint, for that turn of events," he said of his patient's health decline.
"Perhaps the protocol should say, 'administer ketamine and prepare to intubate,' but that's not what it says," said Carney.
"I'm not a proponent of [ketamine] based on my experience. There are other medications available that can do an equally satisfactory job in sedation," he said. "Ketamine has its place. It's a very good pain control agent, and perhaps it's better suited only for that."
Health Department investigation
In 2021, a South Carolina Department of Health and Environmental Control, DHEC, investigation found that neither paramedic involved in Britt's case violated the Emergency Medical Services Act of South Carolina.
However, the department convened an investigative review committee, in October 2022, to conduct a second investigation of the incident.
"The second review came after more information, including bodycam videos, were made available to the agency by law enforcement that were not available for review before," said Ron Aiken, a spokesperson for DHEC.
In 2023, following the second investigation, the department alleged both medics "committed misconduct" during the incident by failing to follow various health protocols, including conducting a Blood Glucose Analysis prior to administering ketamine.
The department made a disciplinary recommendation to suspend each paramedic's certification for a minimum of six months while still allowing them to practice in the field with a reduced certification.
According to DHEC, neither paramedic agreed to the discipline, and both men appealed the agency's decision.
The process, according to DHEC, is currently in the jurisdiction of an Administrative Law Court.
Both men are still certified paramedics in South Carolina.
State and local changes
In South Carolina, and across the country, local agencies are generally responsible for developing their own protocols once a medication like ketamine is approved for them to use.
However, DHEC took additional action to improve how ketamine is used throughout the state.
In October 2022, health leaders sent out a letter to every EMS agency imposing "immediate changes in ketamine protocols and monitoring."
New state standards require 100 percent of ketamine cases to be individually reviewed and submitted to the state.
"I think [deciding to take a closer look at ketamine] was a culmination of things, a lot of which is related to the publicity about it," said Dr. Ed DesChamps, the medical director of the Bureau of Emergency Medical Services at DHEC. "I hope to find nothing, but if there are problems, I would much rather find them than someone else find them," he said.
DesChamps said the agency started collecting data, but "significant changes in the Division of EMS personnel" has caused a "disruption in the collation and review of the data."
Scripps News found Charleston County, which was or is named as a defendant in at least four ketamine-related lawsuits, also made some changes to its ketamine protocols since 2019.
Updated protocols now say, "if the patient is safely restrained by law enforcement ... and there is no risk to patient safety ... chemical sedation is not indicated."
Since 2019, Charleston County's use of ketamine for behavioral reasons decreased from 104 times in 2019 to 11 times in 2022.
National changes
The National Association of EMS Physicians, a group that provides education and resources to thousands of emergency medical professionals nationwide, also took steps to clarify when it is appropriate for paramedics to administer ketamine.
In 2021, the group updated its 2017 position statement on patient restraint, emphasizing the importance of protecting "agitated, combative, and violent patients from injuring themselves while simultaneously protecting the public and emergency responders from injury."
"In these severely impaired patients," the paper said, "rapid pharmacologic management/sedation" may prevent adverse, life-threatening conditions, and "maximize patient safety."
The group referred to the use of ketamine and other medications as an "effective method for protecting the violent or combative patient from self-injury."
In 2017, the medications were described by NAEMSP as an "effective and safe" method for protecting a patient from self-injury.
Scripps News asked NAEMSP’s then-president, Michael Levy, about the subtle removal of the word "safe."
"The word safe is implicit through the entire document," said Levy. "The document describes the safe way to provide care for these patients. Safety is fundamental to the document itself," he said.
The position statement now emphasizes that medics should use the least restrictive method of restraint and that no medic should use ketamine to "facilitate an arrest."
Levy said medics who can communicate with an agitated person should use a "stepwise" approach to de-escalate a situation before moving directly to chemical intervention as a method of calming them.